NURS6512 Week 1: Quiz
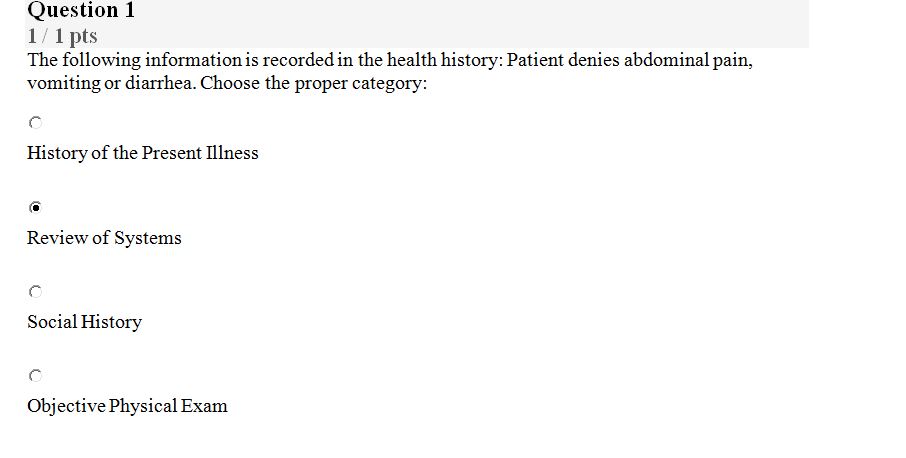
Question 1
1 / 1 pts
The following information is recorded in the health history: Patient denies abdominal pain, vomiting or diarrhea. Choose the proper category:
History of the Present Illness
Review of Systems
Social History
Objective Physical Exa
Question 2
1 / 1 pts
Good patient outcomes can be reflected by which of the following? Select all possible answers.
Gender bias
Health equity
Racism
Cultural humility
Question 3
1 / 1 pts
A unilateral lymph node enlarged, fixed, and hard would be considered:
An abnormal finding
A definite sign of malignancy
A sign of infection
A normal finding
Question 4
1 / 1 pts
Which of the following helps evaluate thyroid function during the Review of Systems?
Increase in size of the thyroid gland
Hoarseness
Intolerance to temperature and sweating
Increase in thirst and urination
Question 5
0 / 1 pts
Health promotion of the older adult, 65 years and older, should include all of the following EXCEPT:
Life expectancy
Treatment feasibility
Testing present allergies
Future comfort measures
Question 6
1 / 1 pts
During an office visit, a 22-year-old female complains of 10 days of vaginal itching, dysuria, and dyspareunia. She is sexually active with the same partner for the last 7 months. She takes no medications, is positive for vaping use, and not sure of her last period. From the following, choose the MOST appropriate element of the focus of the physical assessment for this patient.
Perform a complete Review of Systems.
Instruct the patient about safe sex.
Perform an abdominal and vaginal exam.
Prescribe antibiotic therapy for patient and partner.
Question 7
1 / 1 pts
A 19-year-old male presents with a chief complaint of vomiting and diarrhea for the last 48 hours. Which component of the HPI did the patient provide in the chief complaint?
Location
Character
Modifying factors
Duration
Question 8
1 / 1 pts
During an office visit, a female patient examination reveals bilateral CVA (costovertebral angles) tenderness. Choose a possible differential from the following:
Gallstones
Pyelonephritis
Appendicitis
Pelvic Inflammatory disease
Question 9
1 / 1 pts
A 70-year-old patient with a well-known history of hypertension and renal disease comes to clinic with complaints of new onsets of palpitations and tiredness with activity. The APRN should:
Ask about history of the present illness using OLDCARTS.
Assess CV and pulmonary system.
Perform a head-to-toe exam.
Ask the patient how the new medical problem is affecting his ADLs.
Question 10
1 / 1 pts
When reading a SOAP note, which of the following is incorrectly documented on the physical exam:
Abdominal rash
Constipation
Auscultated peri-umbilical bruit
Left lower quadrant surgical scar. More quizes for this course
Answer Guide:
Unlock the Full Solution Now – Click to Get All Answers!”
NURS6512 Week 1: Quiz